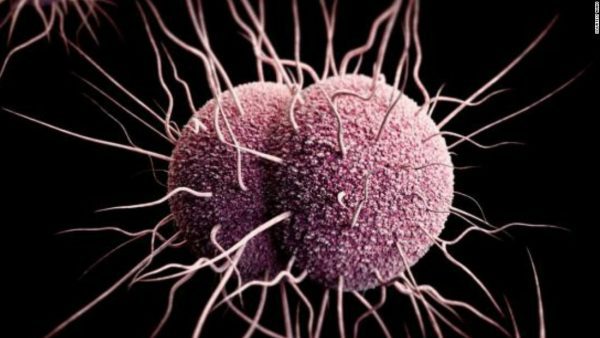
Experts have warned that it is only a matter of time before last-resort antibiotics will be powerless to halt the spread of gonorrhoea. The sexually-transmitted infection affects an estimated 78 million people each year and disproportionately affects women, leading to pelvic inflammatory disease, ectopic pregnancy and infertility, as well as increasing the risk of HIV. At least three people – in France, Japan and Spain – are infected with an untreatable strain of the disease, which they may have spread to others through sex, the World Health Organisation has said.
Teodora Wi, a human reproduction specialist at the Geneva-based UN health agency, said:
“Gonorrhoea is a very smart bug. Every time you introduce a new type of antibiotic to treat it, this bug develops resistance to it.”
Talking of the three cases, she added:
“These cases may just be the tip of the iceberg, since systems to diagnose and report untreatable infections are lacking in lower-income countries where gonorrhoea is actually more common.”
A WHO study found that from 2009 to 2014 there was widespread resistance to the first-line medicine ciprofloxacin, increasing resistance to another antibiotic drugs called azithromycin, and the emergence of resistance to last-resort treatments known as extended-spectrum cephalosporins (ESCs).
In most countries, ESCs are now the only single antibiotics still effective against gonorrhoea, but resistance to them has already been reported in 50 countries. Ms Wi said:
“Currently we’re still using this antibiotic and, in a matter of years, this antibiotic will not be useful anymore to treat gonorrhoea. We need to have new drugs or new development of drugs. It takes years to develop new drugs for gonorrhoea so at the moment we need to prepare for that time, to have that new drug in the pipeline so that, in a few years’ time, we have something to replace the current treatment.”
Only three potential new gonorrhoea drugs are in that pipeline, however and there is no guarantee that they will make it through final-stage trials. One of the problems in diagnosing gonorrhoea is that there is no affordable, rapid diagnostic test for the infection. Many of those infected do not have symptoms and remain undiagnosed and untreated.
Meanwhile, when patients do have symptoms, doctors often assume it is gonorrhoea and prescribe antibiotics, even though patients may be suffering from something else. This increases antibiotic resistance against gonorrhoea as well as other bacterial diseases.
Dr Marc Sprenger, director of Antimicrobial Resistance at WHO, said:
“To control gonorrhoea, we need new tools and systems for better prevention, treatment, earlier diagnosis, and more complete tracking and reporting of new infections, antibiotic use, resistance and treatment failures.”
“Specifically, we need new antibiotics, as well as rapid, accurate, point-of-care diagnostic tests – ideally, ones that can predict which antibiotics will work on that particular infection – and longer term, a vaccine to prevent gonorrhoea.”